Introduction
Acute chest syndrome (ACS) is the 2 nd most common cause of hospitalization and a major cause of mortality in sickle cell disease (SCD). ACS commonly occurs during a hospitalization for a vaso-occlusive crisis (VOC) when the combination of chest wall pain and intravenous opioids may lead to hypoventilation and atelectasis. Incentive spirometry may prevent ACS by encouraging patients to take deep breaths to reduce atelectasis and improve oxygenation, but requires active participation by an awake patient. Non-invasive bi-level positive airway pressure [BiPAP] provides positive pressure breaths via a mask to improve ventilation and prevent atelectasis during sleep. Hospitalized pediatric SCD patients who were at risk for ACS have used nocturnal BiPAP for ACS prevention on the Boston Medical Center (BMC) general pediatric unit since February 2017. In January 2023, BMC instituted the use of nocturnal BiPAP in hospitalized adult patients with SCD who are at high risk for ACS.
Methods
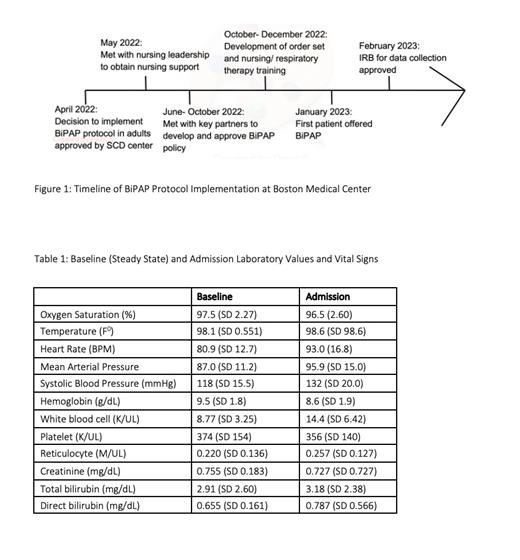
This is a prospective observational cohort study to examine the safety, acceptability, and tolerability of BiPAP in high-risk adult patients with SCD hospitalized with a VOC. Criteria for increased ACS risk included: 1) Oxygen saturation < 94% on room air at presentation; 2) History of pulmonary hypertension diagnosed by right heart catheterization; 3) Known obstructive sleep apnea (OSA) not currently treated with positive airway pressure; 4) Prior severe ACS requiring invasive or non-invasive ventilation, high-flow oxygen, and/or exchange transfusion; or 5) History of fat emboli syndrome. Exclusion criteria were: 1) OSA being treated with outpatient positive airway pressure, 2) Surgery within the last 30 days, 3) Direct admission to the intensive care unit (ICU). Manual chart extraction was used to collect patient demographic data, medical history, symptoms, vital signs, chest radiography, laboratory data, indications for BiPAP use, and acceptability and use of BiPAP.
Results
BiPAP was offered during 38 hospitalizations to 25 individual patients (14 (56%) female) between February and July 2023. The mean age was 35.8 years (SD 10.2); 16 (64%) were HbSS, 8 (32%) HbSC and 1 (4%) HbS-β 0. Nineteen patients (76%) were using >1 SCD-modifying therapy; 16 (64%) reported hydroxyurea use. ACS was present on admission in 7 hospitalizations.
Patients agreed to try BiPAP in 22/38 hospitalizations (58%) and BiPAP was used for 1 night in 3 hospitalizations, 2 nights in 3 hospitalizations and more than 2 nights in 7 hospitalizations. In 9/22 hospitalizations, attempts at BiPAP use were unsuccessful.
Of the 38 hospitalizations in which BiPAP was offered, 3 patients who did not use BiPAP were transferred to the ICU, 2 for ACS and 1 for ketamine infusion for pain that was refractory to high doses of opioids. Three episodes of ACS developed after admission to the hospital: 2 when BiPAP use had not been attempted and 1 when BiPAP was used for 6 days. Blood transfusions were administered during 7 hospitalizations; 5 of which BiPAP was not used. No deaths occurred during this study period.
No adverse events were directly attributable to this novel use of BiPAP for ACS prevention. In the 22 encounters where BiPAP use was attempted, four patients noted difficulties with the continuous airflow and feeling suffocated, one reported lightheadedness. One patient who used BiPAP developed oral pain related to periodontal disease.
Conclusion
Medically stable, adult hospitalized patients with SCD and VOC were willing to try BiPAP to prevent the development of ACS. In 13/22 (59%) BiPAP was tolerated for >1 one night with no adverse events noted. Future directions include optimizing implementation and studying the efficacy of this intervention.
Disclosures
Ribeil:Bluebird Bio: Other: shareholder ; Moderna: Consultancy; Akirabio: Consultancy. Cohen:Forma Therapeutics: Consultancy, Other: member of a one-time advisory board meeting about clinical trial endpoints ; Sanofi: Other: Member of an independent data safety monitoring board. Klings:Vertex: Other: Advisory board for gene therapy; Bayer: Consultancy, Other: clinical trial support; United Therapeutics: Consultancy, Other: Clinical trial support; CSL Behring: Other: safety review committee for Phase 1 trial; Novo Nordisk: Consultancy, Other: clinical trial support; Forma: Consultancy, Other: clinical trial support; Novartis: Consultancy, Other: Clinical trial support.